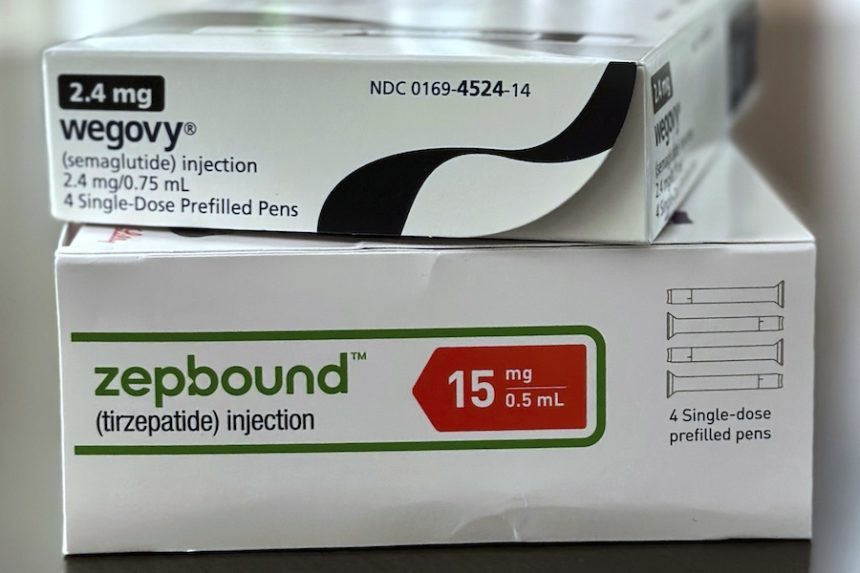
Wegovy and Zepbound, two well-known medicines for obesity, are becoming less expensive, but consistent availability to the medications is still difficult.
Many patients cannot afford the drugs, which still cost about $500 a month for those without insurance. Additionally, coverage is still inconsistent even for those who have insurance.
Matt Maciejewski, a professor at Duke University who specializes in obesity treatment coverage, stated that while the drugs should be accessible, the concern is how much they will cost and whether patients can afford them.
Though there is hope that costs may decrease further in the future, doctors say the current situation encourages them to be innovative in how they treat patients.
The medications are still in great demand.
GLP-1 receptor agonists, a class of obesity drugs that have become quite popular, include Wegovy and Zepbound.
During the first quarter of this year, Zepbound generated $2.3 billion in sales in the United States, making it one of Eli Lilly’s top-selling medications.
According to Novo Nordisk, Wegovy generated close to $1.9 billion in sales during the first quarter of this year and has over 200,000 prescriptions written each week in the United States.Some people’s insurance coverage is growing.
According to Mercer, a benefits expert, more companies with 500 or more workers are covering their employees’ and their families’ injection medication coverage.
Additionally, according to Novo, 85% of its insured patients in the US spend $25 or less a month.
Additionally, some diabetic patients are eligible for coverage of Novo and Lilly’s approved GLP-1 medications, Ozempic and Mounjaro.
However, neither Medicare, the federal program primarily for those 65 and older, nor the majority of state and federally sponsored Medicaid programs pay the medications for obesity.
According to Dr. Beverly Tchang, even insurance plans that cover the medications frequently only cover a fraction of the expenditure, leaving patients vulnerable to monthly expenses of hundreds of dollars.
Pharmaceutical companies provide some support, but it may not be sufficient to cover these out-of-pocket expenses.
According to Tchang, a physician in New York who advises Novo and Lilly for a fee, coverage is not the same as access.
However, coverage is still patchy.
Employers and other bill-payers are concerned about medications that many people may use for an extended period of time.
Because of the cost, some large employers have stopped covering the medications. As they bargain with the pharmaceutical companies, pharmacy benefit managers, or PBMs, are now beginning to favor one brand over another.
On July 1, Zepbound was removed from the national formulary, or list of approved medications, by CVS Health, one of the biggest PBMs in the country, in favor of Wegovy.
For a number of patients, many of whom used Zepbound because it reduced their nausea, Tchang was compelled to come up with an alternative therapeutic strategy.Before they come, potential patients are sent a video link from Dr. Courtney Younglove’s office that demonstrates how to check their insurer’s website for coverage of the medications.
Then, according to the doctor in Overland Park, Kansas, some of them just cancel their appointment because they lack insurance.
The sale of less expensive compounded medications continues.
When Wegovy and Zepbound were in short supply, compounding pharmacies and other organizations were permitted to produce cheaper, off-brand versions of the medications. However, earlier this year, the U.S. Food and Drug Administration declared the shortage to be over.
The compounded versions should have stopped at that point, but there is an exception: when a medication is customized for a patient, some compounding is allowed.The medication semaglutide, which is the active ingredient in Wegovy, is available in compounded doses from Hims & Hers Health, which allow patients control adverse effects by varying dosage levels. According to Hims, these programs start at $165 per month for a full year, and clients must pay in full up advance.
It’s a controversial topic. In an attempt to prevent pharmacies and telehealth businesses from offering compounded versions of their medications, Eli Lilly has filed lawsuits against them.
Due of Wegovy’s continued compounding, Novo recently terminated a brief collaboration with Hims to sell the telehealth startup. Novo claims that because the chemicals in the compounded forms of its medication are produced by overseas vendors who are not subject to US regulatory oversight, patient safety is at risk.
According to Hims, it verifies that every ingredient satisfies American safety and quality requirements. In order to confirm that a drug’s strength is appropriately labeled, a third-party lab is also used.
Prices have decreased.
Both pharmaceutical companies are offering the majority of their doses to uninsured patients for about $500 per month, which is several hundred dollars cheaper than some of the original costs.
Nevertheless, such cost would account for almost 14% of the $43,000 average annual income per person in the United States.
Over time, several variables may cause prices to decline. Both businesses are creating pill forms of their therapies. In the coming year or so, such might be available on the market, which could result in lower costs for the more traditional injectable dosages.
According to Younglove, some of her patients save up to 15% by ordering their medications from a Canadian pharmacy. Before the Canadians lowered their costs, they used to purchase them from an Israeli pharmacy.
She claims that the launch of pill versions and competition like this will put pressure on U.S. prices.
Price wars, in my opinion, will drive it down, she said. I believe we are just getting started. I’m hopeful.