Research on mice and human cells may have consequences for other lysosomal storage diseases.
LOTS is a hereditary condition brought on by a mutation in the HEXAgene that results in a lack of an enzyme essential for the breakdown of GM2 ganglioside, a fatty material in the brain. This fatty material accumulates and destroys brain and spinal cord nerve cells. The severity of the condition and the age at which it first appears are influenced by the quantity of enzyme that the body is currently producing. Scientists were able to delay the onset of symptoms, boost the activity of the enzyme beta-hexosaminidase A, and considerably improve lifespan in the mouse model by applying the repair to the HEXAgene.
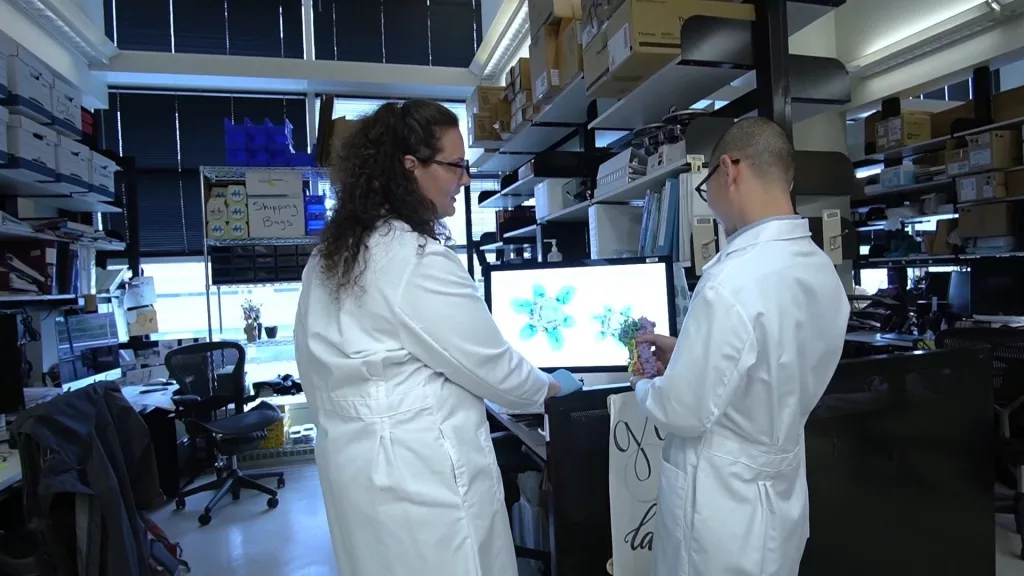
A small correction will have a big impact with LOTS. According to research author Dr. Richard Proia of the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health, this editing may only need to raise enzyme activity by roughly 10% to prevent symptoms from worsening and enhance their quality of life. We have discovered that it is possible to open the door to greater enzyme activity; the next step is to determine how to accomplish this in a human.
This degree of pre-clinical research, according to scientists, has set the groundwork for testing on human subjects. There are now about 25 participants in an ongoing trial at the NIH Clinical Center in Bethesda, Maryland, and researchers estimate that LOTS affects roughly 500 people worldwide. One person, who is special because they have two copies of the mutant gene, supplied the human cells used in this study.
According to research author Dr. Cynthia Tifft of NIH’s National Human Genome Research Institute, “I have never encountered a study participant who was so eager and enthusiastic to be part of the scientific process.” Working with someone who maintains their enthusiasm and optimism despite this disorder depriving them of bodily control is encouraging. Knowing that the work we’re doing counts inspires me every day.
Although there is currently no cure or effective treatment for the condition, researchers think they are moving in the right direction. Future research will look into the most effective methods of delivering the genetic edit to the brain and central nervous system. Adeno-associated viruses (AAVs) are a technique utilized in numerous other gene-editing investigations to transfer DNA modifications to specific cells. Many individuals who may already have developed antibodies against some of the usual virus particles used for the delivery method have problems with AAVs, which are non-enveloped viruses that can be created as a delivery vehicle. AAV vectors may need to be improved in the area of blood-brain barrier crossing, which presents another challenge.
Because other types of Tay-Sachs disease manifest more abruptly, researchers have focused their study on LOTS. The disorder’s infantile form is often identified in the first three to six months of life and is lethal by the time a child is four to five years old. While infants have no activity in the beta-hexosaminidase A enzyme, people with LOTS have an activity level of 4-6%, which speeds up the accumulation of harmful GM2 ganglioside. Teenagers who are diagnosed with the disease’s juvenile version frequently pass away.
Certain populations, such as the Cajun community in Louisiana, the Old Order Amish community in Pennsylvania, some French-Canadian communities in Quebec, and Eastern and Central European Jewish communities (Ashkenazi Jews), are known to have higher rates of mutations in the HEXA gene that cause Tay-Sachs disease. Pregnant women and their partners in the US are frequently offered a blood test to determine whether they are carriers of the Tay-Sachs disease-causing HEXA gene mutation.
The NIDDK, a division of the NIH, carries out and funds clinical and scientific research as well as research training on some of the most prevalent, severe, and incapacitating illnesses that Americans face. The Institute’s research interests include renal, urologic, and hematologic illnesses; obesity, nutrition, and digestive disorders; and diabetes and other endocrine and metabolic disorders. To learn more, go to https://www.niddk.nih.gov/.